Setting up your birth space is one creative way that you can prepare for a comfortable experience!
Bringing a child into the world is a momentous occasion, and creating the right ambiance can enhance the experience and make it even more memorable. Whether you're at a birthing center, a hospital room, or the comfort of your own home, setting the right mood through sensory elements can have a profound impact on the birthing experience.
Let's explore some items that can help create a serene, calming, and soothing atmosphere during this beautiful journey. Doulas, step up your game and invest in some of these items for your birth bag!
These are items that I have in my own doula bag, have recommended to those I’ve supported through birth, or educated in my classes. Some of these items are living in my home!
This blogpost may contain affiliate links, which means I make a small amount if you make a purchase, without you paying more for the item.
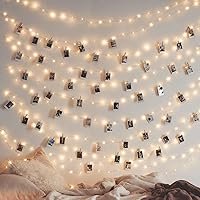
1. Electric Candles and Fairy Lights:
Electric candles and fairy lights are perfect for adding a gentle, warm glow to the room. The soft flickering of the electric tea light candles mimics real candlelight, creating a cozy and calming environment. Fairy lights can be draped around the room or hung in a strategic manner to add a touch of magic and charm, and are great for Doulas that want to have these on hand for their clients. If you want to go all out, Twinkle Star comes with 66ft of flexible copper wire, a remote, and are waterproof! You might even like this rose quartz lamp or amethyst lamp.
2. Aromatherapy and Diffuser:
Aromatherapy is a wonderful way to engage the sense of smell and promote relaxation. Using essential oils like lavender, chamomile, or frankincense in a diffuser can fill the room with calming scents, alleviating stress and anxiety for both the expectant mother and her support team. This set comes with the four most used oils for birthing. This DoTerra set is quality. If you want the benefits of clary sage, you will have to order separately. Just make sure that everyone in the room is ok with essential oils, as some people are sensitive and can react to them.
3. Salt Lamp:
Salt lamps not only offer a soothing, warm glow but also help purify the air. The subtle lighting and the gentle hum of negative ions released by the salt lamp create a tranquil atmosphere that promotes relaxation and a sense of peace. The plug-in salt lamp night lights are great for a warm glow, easy to set up. If you want to go big, you can use these salt lamp fairy lights!
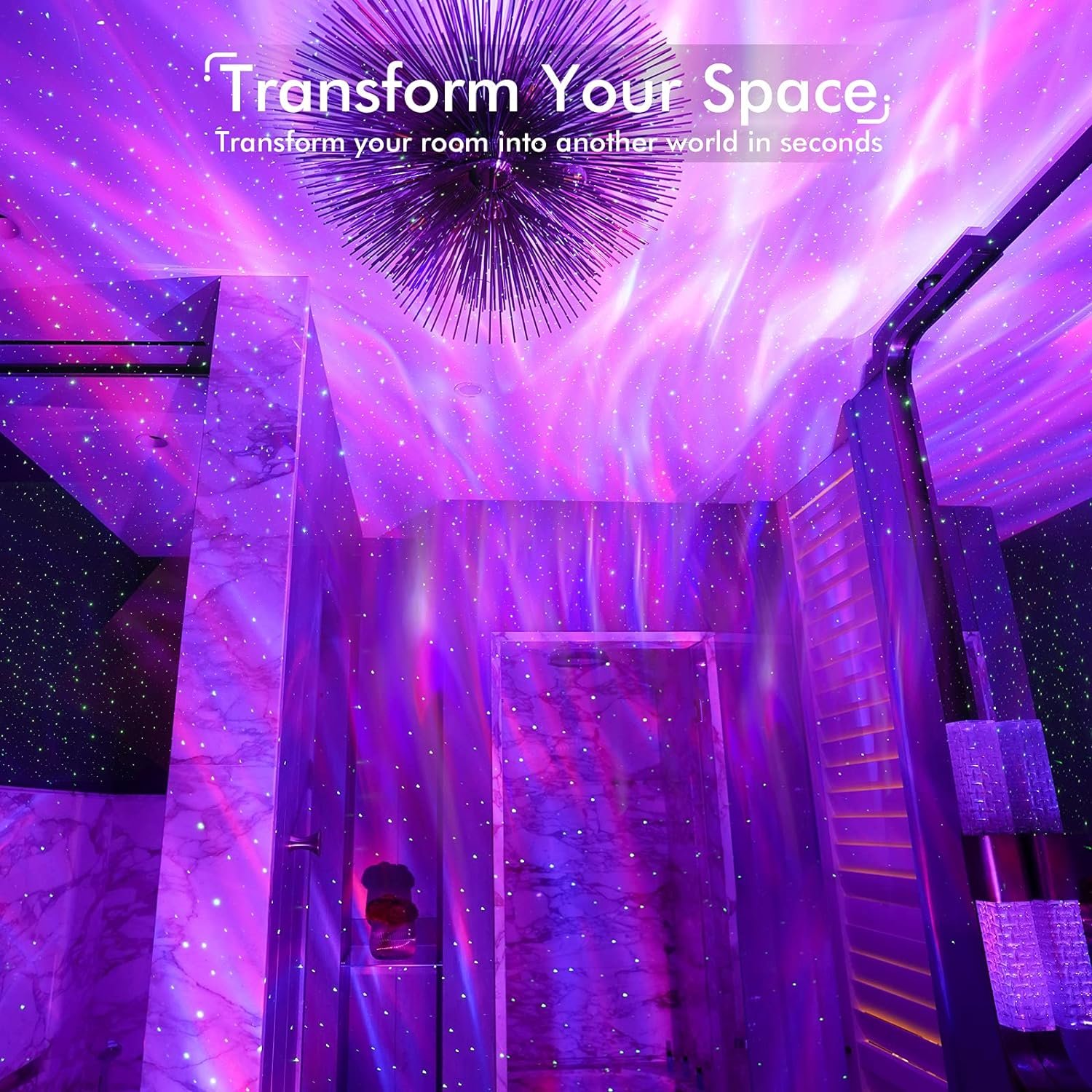
4. Star Galaxy Projector Lights:
Transform the room into a celestial wonderland with a star galaxy projector light. These lights project a mesmerizing display of stars and galaxies on the ceiling, providing a serene and dreamy atmosphere that can help distract from any discomfort and keep the mind at ease. Bliss Lights is one that we have used and loved. Doulas, if you keep this in your birth bag… you’ll definitely be stepping up your game.
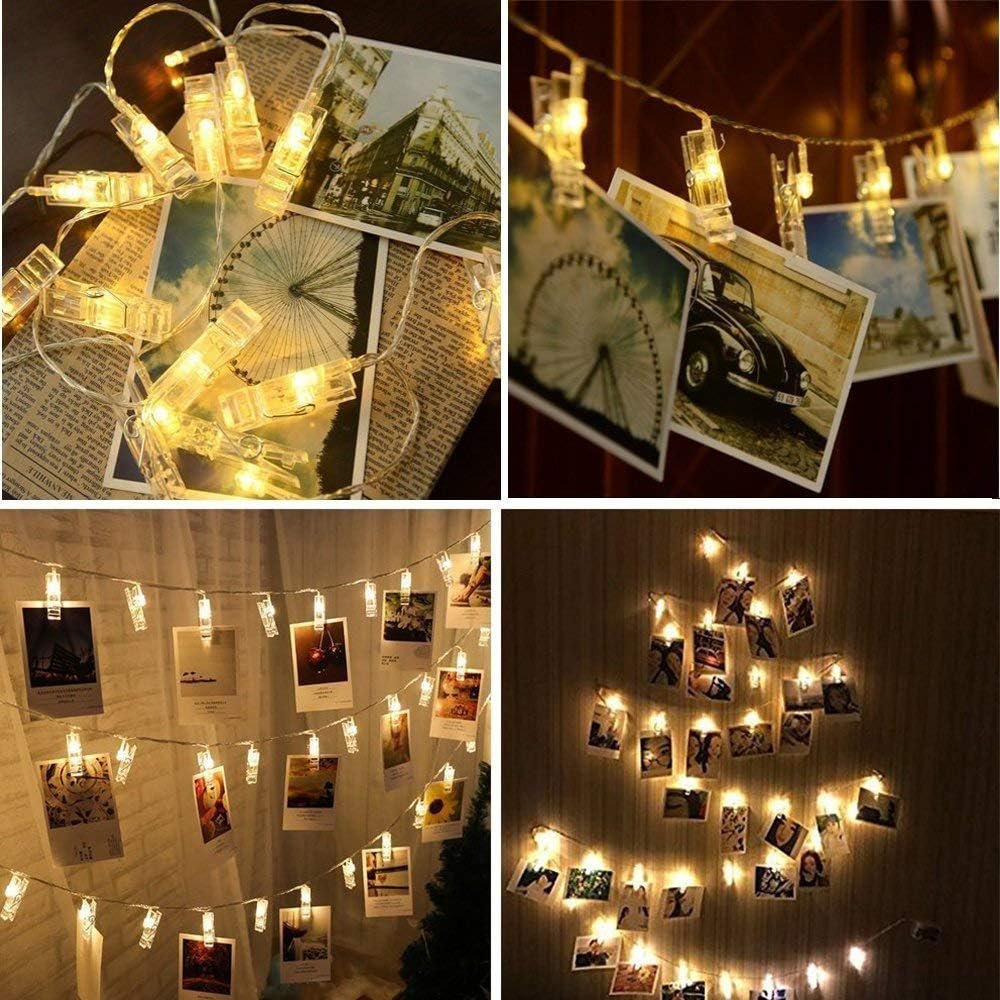
5. Photo Frames With Cherished Memories:
Display framed photos of cherished memories or loved ones to evoke positive emotions and create a sense of comfort and support. An accordion style stand-up frame is one way to easily keep a few beloved pictures in view, (such as baby’s ultrasound pic) to use as a focal point or to display your favorite affirmations. I’ve even seen a creative setup where pictures were hung with a felt board message displayed! A combo fairy light + picture (with clips) is fun!
6. Bluetooth Speaker:
Music can be incredibly therapeutic during labor and birth. Utilize a Bluetooth speaker to play calming tunes, nature sounds, hypnobirthing tracks, or even a carefully curated playlist that resonates with your preferences. Music can help reduce stress, elevate mood, and create a positive ambiance. The Ankar waterproof speaker is great for obvious reasons.
7. Calming Soundscape Machine:
Incorporate a sound machine that plays calming sounds like ocean waves, rainforest, or white noise to create a peaceful auditory backdrop. This one is great, has a dim light, and can be used for baby afterwards! This soft light meditation machine is a great option.
8. Soft, Comforting Fabrics:
Incorporate soft blankets, cushions, and pillows made from natural, comforting fabrics like cotton or fleece. These textures can provide physical comfort and contribute to a cozy and inviting birth environment. Everlasting Comfort has a great Minky Faux that helps to hide possible staining. Cozy Earth blankets have graced many a hospital bed, and are great for postpartum too.
9. Comfortable Seating:
Provide options for alternative birthing positions to encourage movement and ease of labor, like birthing stools, THE CUB (best ever) and birth balls. Read more about birth balls HERE. If you want to go all out, Cushion Lab makes a cozy seat that people have used on the rocker in the hospital during and after birth.
10. Visual Birth Affirmations:
Positive affirmations can help maintain a calm and confident mindset during labor. Create affirmation cards or print out inspiring quotes that resonate with you. Place them around your birthing space as a constant source of motivation and reassurance.
11. Essential Oil Rollerballs:
Offer the expectant mother the option to use essential oil rollerballs infused with specific essential oils for relaxation or pain relief. The act of applying these oils can also be comforting and provide a moment for mindfulness. Clary Sage, Peppermint for nausea, Citrus for uplifting, and lavender for comfort/anxiety. Read more about the evidence on aromatherapy for birth.
12. Gentle Massage Tools:
Incorporate gentle massage tools like a massage roller, a vibrating peanut ball massager, a non-vibrating peanut, or a handheld massager such as THIS or THIS, to help relax tense muscles and provide comfort during contractions. The soothing touch can be incredibly comforting.
13. Herbal Teas and Infusions:
Offer a selection of herbal teas or infusions that promote relaxation and hydration. Warm beverages can be soothing and comforting, contributing to a peaceful birthing environment.
Creating the right mood for a birth experience is all about embracing elements that engage the senses and promote relaxation and tranquility. By incorporating electric candles, fairy lights, aromatherapy, salt lamps, star galaxy projectors, bluetooth speakers, and other comforting elements, you can enhance the birthing journey and ensure a serene and memorable experience for all.
ENJOY!!!
Disclaimer: The content of this document, such as copy, images, graphics and any other material contained on this website ("Content") is for informational purposes only and does not constitute medical advice; the Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of a physician, midwife, or other qualified health provider with any questions you may have regarding any medical condition. Never disregard legitimate medical advice or delay in seeking it because of something you have read on this document. In the event of a medical emergency, call your doctor or 911 immediately. This company, website or document does not recommend or endorse any specific tests, physicians, procedures, opinions, or other information that may be mentioned on this site. Reliance on any information provided by this document, without consulting medical advice or research is solely at your own risk.